Insights to improve benefits offerings and spend for diabetes and behavioral health

Rising healthcare costs, provider network consolidation, and inflation have all contributed to the increasing financial burden on patients and employers. While there is no one-size-fits-all solution, employers play a critical role in helping members overcome some of these challenges. To help inform decisions, many companies now leverage health data and analytics to evaluate and improve benefits offerings and spend in areas like diabetes management and behavioral health. At The Conference Board's Annual Employee Health Care Conference earlier this year, we sat down with Trane Technologies and Eaton Corporation and covered various healthcare affordability and access challenges and explored analytics strategies they’ve implemented to address barriers to care.
Diabetes management with Eaton Corporation
Healthcare affordability continues to be top of mind for payers, as stakeholders across the healthcare industry grapple with the rising cost of care. As part of our payer trends webinar, we wanted to dig into the data and see what factors were driving cost increases. Using our MarketScan commercial claims data, we analyzed total medical and pharmacy claim costs for the last five years. We found that year-over-year, prescription drugs are up almost 10% and facility charges, both inpatient and outpatient, are up 13%.
In 2020, Eaton Corporation pursued an innovative plan to help their employees contend with the cost of diabetic medications in particular. With the goal of increasing medication adherence and lessening the severity of chronic conditions, Eaton made changes to its prescription drug plan to cover all antidiabetic medications, including insulin, at full cost. Eaton then asked their Truven healthcare analytics consultants for help in understanding how the changes impacted diabetes prescription drug utilization, medical cost, disease progression, patient prevalence, and overall trends.
Relying on Truven Health Insights, we observed that Eaton had a growing diabetic patient population, with many new members seeking care after this benefit was rolled out. Certain patient cohorts saw marked improvements in medication adherence and decreases in negative outcomes, such as emergency visits and admissions. Eaton also saw dramatic increases in the use of expensive antidiabetic medications, where price may have previously been a barrier, however this use did not exceed MarketScan® normative data, suggesting that this benefit is not being abused.
Eaton is a prime example of using data to deeply understand employee needs and implement actionable decisions to make healthcare more affordable for patients. This type of analysis helps Eaton prepare for discussions with their C-suite, who want to know whether recently implemented changes to benefits plan design actually had the intended impact.
"When they ask, 'Hey you told us last year that putting this benefit in was going to save us X, have we been able to validate that?' That's where we look to Truven to help create that measurement strategy to evaluate some of the benefits designs and program changes we've made over the years."
– Ethan Rush, Director of US Medical Benefits, Eaton Corporation
Ready to identify savings? Try product tour
Behavioral health with Trane Technologies
Healthcare access is a continuing challenge as the industry works to make care more inclusive, more accessible, and more personalized. Fortunately, over the last few years we’ve seen technology help reduce barriers to care with innovations like telehealth.
We wanted to see how telehealth utilization has changed since the pandemic and if there were any signs of it stopping. With our healthcare analytics, we examined physical and mental health telehealth utilization from the early stages of the pandemic (January 2020) through November 2021 and summarized our findings in a blog.
We discovered telehealth use by behavioral and mental health practitioners accounted for almost 60% of visits in April 2020, far exceeding use by general practitioners (25%). Furthermore, behavioral telehealth utilization persisted; accounting for 40% of visits in November 2021.
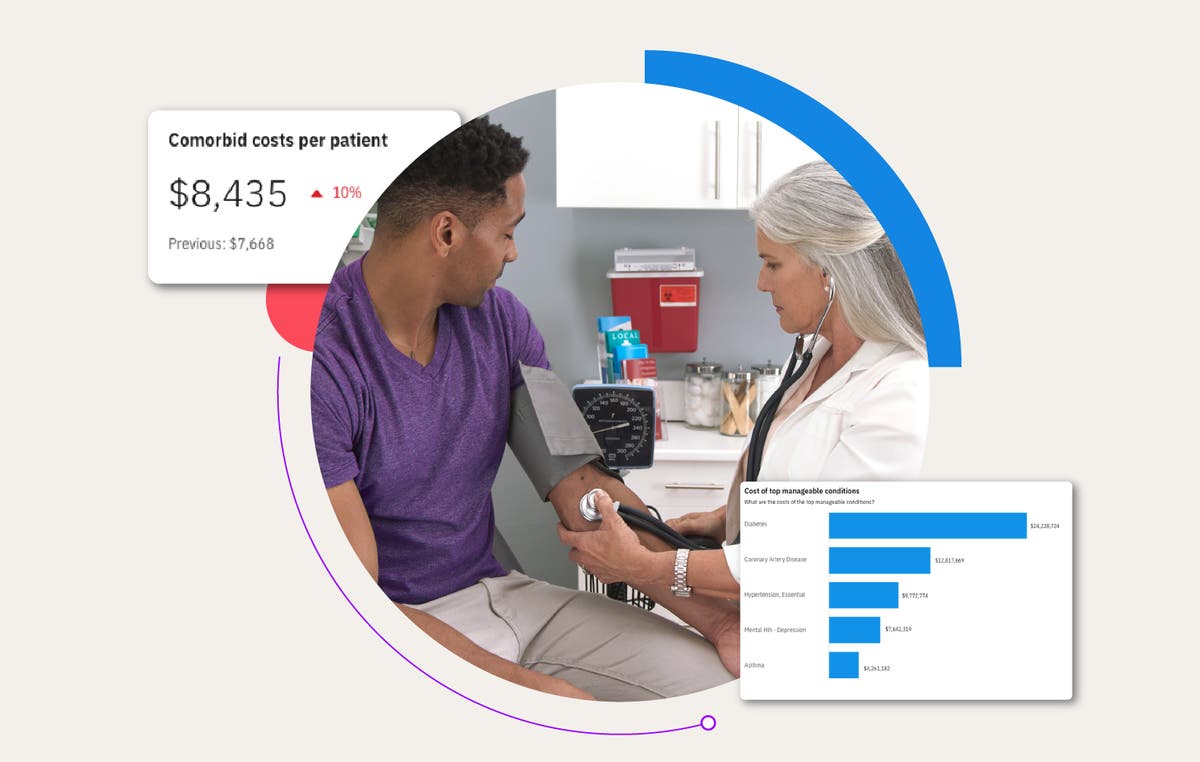
Acknowledging the impact that the pandemic had on its own workforce, Trane Technologies wanted to examine the impacts of mental health and substance abuse on their employee population. Trane Technologies took action and implemented an internal survey to compare the results alongside benchmarking data. Their next step was to work with our team to get an expanded view of the impact. Once again, our team relied on Health Insights to help Trane Technologies assess the current impact of mental health on their members, as well as the resources available to them. The findings were striking:
- 94% of members with a Mental Health and Substance Abuse (MHSA) episode have at least one comorbidity
- 2X higher overall cost of care for members with MHSA episodes compared to those without
- Substance abuse care drove highest percentage of out-of-network costs
- Discovered many members with mental health referrals and indicators, but no treatment
After uncovering these critical insights, the Trane Technologies team jumped into action focusing on improving employee communications, making resources more accessible to members in need, and leveraging dashboards to create measurement strategies that assess efficacy. Looking ahead, Trane Technologies hopes to continue improving on overall condition management and using their health data to inform decisions and next steps.
Related Articles
From data to decisions: How Truven is shaping the future of healthcare
2024 has been a landmark year for Truven, filled with significant milestones and...
By Marcy Tatsch | 4 min. read

Healthcare price transparency: What it means for members, employers, and health plans
In today’s digital world, consumers can shop for goods and services with just a few...
By Bryan Briegel | 5 min. read
How healthcare analytics help employers reduce costs and improve employee health
Year after year, employers grapple with rising healthcare costs that feel beyond...
By Jennifer Huyck | 4 min. read
Ready for a consultation?
Our team is ready to answer your questions. Let's make smarter health ecosystems, together.
