Optimizing value-based healthcare: 5 strategies for effective provider network management

In today's rapidly evolving American healthcare industry, the collaboration between healthcare providers and payers has never been more crucial. The shared goal? To focus initiatives on improving patient outcomes while simultaneously reducing healthcare costs. As many organizations transition from a strictly fee-for-service model and enter more value-based payment arrangements, advanced healthcare analytics can help surface valuable insights about the cost and quality of care, across factors like payment models, bundled payments, competitive network rates, Accountable Care Organizations (ACOs), or patient-centered medical homes (PCMH). To act on those insights, providers must be able to trust them, making it equally important to adopt a strategic reporting approach around provider insights and reimbursements. Here are five key considerations when building your strategy.
Attribution in healthcare: Who's responsible for what?
Attribution is a critical aspect of value-based healthcare. It involves determining which healthcare provider is responsible for a patient's care and what aspects of care coordination they are responsible for. Attribution comes in many flavors, including who saw the patient the most, who delivered the most healthcare services for a specific condition or chronic disease, or who the patient chose as their primary care provider. A flexible and transparent approach to attribution is a key consideration and starting point in the process.
Aside from gatekeeper models, healthcare providers need to be confident that their methodology accurately attributes patients to their practice before starting an evaluation. They need to understand who is in their “panel” and what care that entails—whether that is total cost of care for a primary care physician or what a specialist physician is responsible for when evaluating an episode of care and the related costs (e.g. endocrinologist treating diabetes).
Industry-accepted healthcare methodologies
The foundation of a robust healthcare network management strategy lies in using trusted methods and reliable data. When available, embedding industry-accepted metrics into arrangements (e.g., HEDIS/NCQA, Pharmacy Quality Alliance, Choosing Wisely, AHRQ) can be instrumental in securing provider support. When an industry standard is not available, such as episodes of care, buy-in and trust can be achieved by implementing a methodology that is well known, has been time tested, and is accepted in the industry by clinicians.
Insights should be supported by trustworthy data sources, such as benchmarks that stakeholders can trust. For example, when renegotiating reimbursement rates, pull in market-level reimbursement benchmarks to advance the conversations. While the machine-readable files (MRFs) introduced under the Transparency in Coverage (TiC) Final Rule offer great promise, the size, usability and accuracy is still being vetted. Presenting reimbursement benchmarks from paid claims in renegotiation conversations can serve as a powerful data point to advocate for fair reimbursement and lower costs.
- Risk-adjusted medical episodes for efficiency scores (including case-mix adjustment, benchmark performance)
- Quality rules for effectiveness scores (including HEDIS, PQA, Choosing Wisely)
- Advanced cohorting for peer group comparison (set thresholds, define specialty, remove outliers, peer group benchmarks, etc.)
- Physician attribution models (In addition to plan assigned/member selected: Imputed PCP, Episodic, Quality Rules, etc.)
- Transparency (Methodology, scoring, attribution, case-mix adjustment, peer selection)
Fair provider peer groups
It is human nature to strive for excellence, especially among providers dedicating their lives to advancing population health and the patients they serve. Fair peer comparisons are critical for effective reporting and accurate insights into provider performance relative to their peers. To foster buy-in from healthcare providers, they must know the industry-standard performance metrics used in evaluations and the peers they are being compared against. While external datasets are important here, identifying true peers within those datasets is critical.
For example, larger provider practices may prefer to be grouped with those of similar size, while smaller practices might need to meet a minimum threshold to be included in analyses. Comparing providers in the same specialty is also key. For example, an internal medicine provider managing cardiovascular patients will undoubtedly approach care differently than a cardiovascular surgeon. These expected differences in cost and practice pattern must be considered to create a fair comparison. Thus, factors like markets, products, rural versus urban settings, and specialties should be included in peer group definitions, so providers see it as a fair, apples to apples, comparison.
Risk adjustment for clinical severity and patient complexity
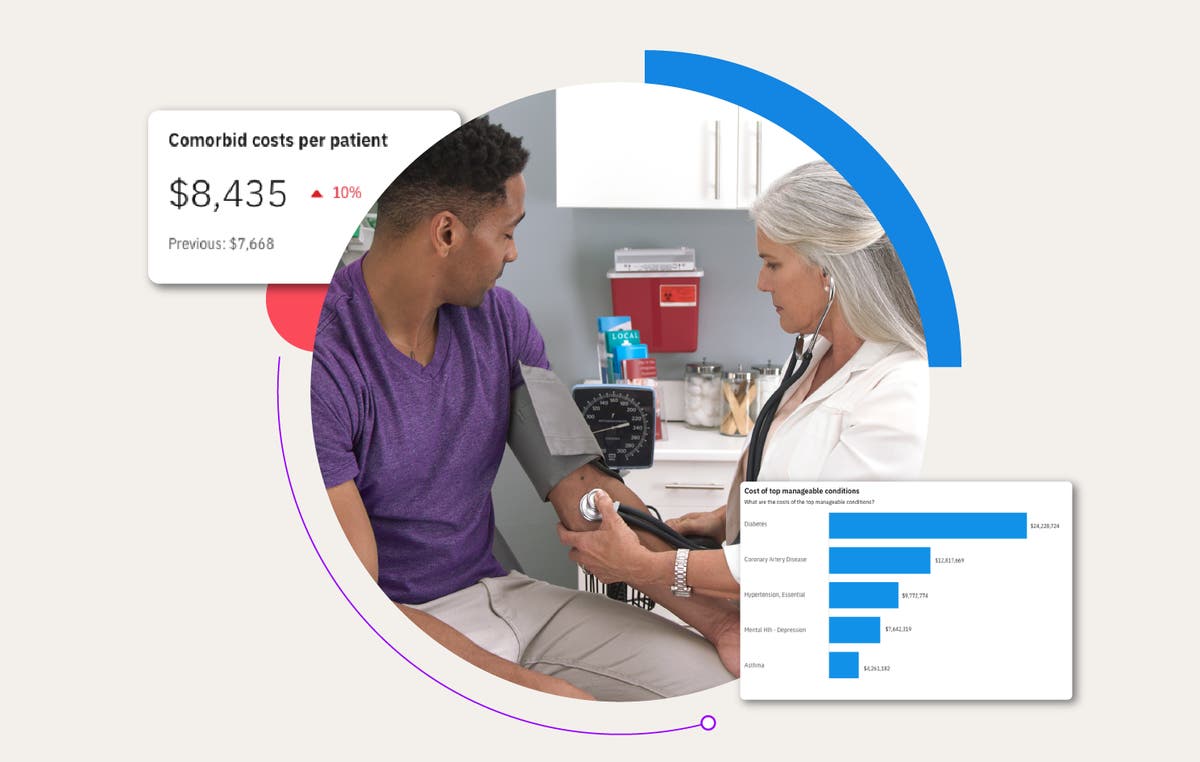
As many business decisions are driven by financial metrics, lowering healthcare costs is a key component in provider reporting across all markets, including Medicaid, Medicare, and Commercial. It's important to show providers their efficiency alongside effectiveness, whether analyzing total cost of care per member per month (PMPM) or episodes of care. However, the common justification – “I cost more because my patients are sicker” – needs to be accounted and adjusted for.
Consider two providers: Provider A treats a patient with Type 2 Diabetes and impaired fasting glucose, while Provider B has a patient with Type 2 Diabetes who also suffers from hypertension and foot ulcers. Provider B requires more resources due to the increased risk and severity in their patient's case. By having a well-defined risk adjustment methodology that considers the risk and severity for each patient episode, providers can be confident they are being held accountable for equitable care.
Transparency of methodology
Trust in evidence-based methodologies is essential, but transparency is what truly builds confidence. Both providers and payers struggle with the “black box” approach to analytics. This can manifest in various ways, from detailed documentation on how episodes of care are constructed, the methodology used for risk and severity adjustment, to the underlying detail behind the scores themselves (e.g., here are all the patients’ gaps in care, how they were attributed to you, their last service date, and status).
Regardless of your physician profiling goals—be they incentive reimbursement, informational, educational, value-based care contracting support, care delivery, network configuration and design—having the methodology, transparency, and provider buy-in and trust to support your organization's process is critical. There are many vital components to a successful profiling effort. Having a strong network strategy in place will drive population health, maximize your return on investment, and ultimately improve your bottom line.
See why more than 190 health plans, employers, and state Medicaid agencies use our proprietary Medical Episode Grouper to compare medical and surgical options and costs in the treatment of diseases and medical conditions.
Conclusion
- Support value-based programs
- Create tiered & high-performance networks
- Create scorecards by ACO, practice or physician
- Compare peer groups by specialty; benchmark performance
- Improve plan performance metrics (i.e., HEDIS, Stars, etc.)
- Negotiate competitive rates leveraging paid claims reimbursement benchmarks
- Engage providers with patient action lists
Successfully navigating value-based healthcare requires a team effort across providers, insurers, and patients. By using strategies like clear attribution, reliable data, fair comparisons, adjusting for clinical complexity, and prioritizing transparency, we can create a healthcare system that is both efficient and fair. Embracing these methods will help providers deliver high-quality care, improve health outcomes, and lower costs. Moving forward, having open conversations and building trust in our approaches will be essential for achieving our goal of better patient health and sustainable healthcare. Together, we can improve patient experiences and achieve better health outcomes for all.
Related Articles

Healthcare analytics to identify the right member, the right intervention, at the right time
Managing the health of your member population is an important responsibility, but...
By Carrie Frederick | 5 min. read

Unlocking real-time insights: how on-demand analytics reduces latency for faster decision-making
When it comes to data-driven decision making, analytic latency can have a major...
By Kristen Hutchins | 5 min. read
How healthcare analytics help employers reduce costs and improve employee health
Year after year, employers grapple with rising healthcare costs that feel beyond...
By Jennifer Huyck | 4 min. read
Ready for a consultation?
Our team is ready to answer your questions. Let's make smarter health ecosystems, together.
