Health equity solutions: You can’t go with your gut

This is intuitive: Individuals experiencing social and economic disadvantage, including racial and ethnic inequities, face greater challenges accessing healthcare. They also experience poorer health outcomes.
Data supports this, and these factors are well-understood social determinants of health (SDoH).
This might not be intuitive: Loneliness and social isolation can also have significant, negative impact on health.
The data supports this, too. But without looking at all the data, the latter group could remain invisible.
We need data to track and measure. And further, we need collaboration with a variety of people and organizations to ensure our health equity goals and strategies are sound. Different industries and organizations receive different data. And that data is critical in understanding a population and how to help.
Three Steps
To best address your population’s SDoH and overcome related health inequities, consider first how to define and communicate your specific goals and principles for promoting equity. Then spend as much time focusing on ways to measure your successes. Finally, create collaborations with key stakeholders.
Step 1: Start with principles related to health equity
For all stakeholders, some overarching goals for achieving health equity include:
- Ensuring that all people live in thriving communities, where they can access social services, healthcare and food pantries, and other health-promoting resources, for example
- Evaluating systems, policies and programs for their impact on equity, to ensure that they cause no harm, nor exacerbate existing harms, for example
- Ensuring patients have the power, agency, opportunities, and the right resources to achieve their optimal health. Examples include having patient navigators, advocates and support for caregivers, for example, to navigate the complexities of a health system
- Ensuring providers have the right resources and training. These include tools to help them build competencies, consciousness and compassion to confront inequities.
- Developing processes so that key organizations and populations can work collaboratively
With the right combination of data, technology and collaboration, organizations can use analytics to identify areas for improvement from their population health data. But population health data only shows you a piece of the puzzle. We can help you merge your datasets with publicly available data, helping unlock more insights into your population and their needs.
Step 2: Select measurable criteria to evaluate success.
Measurement starts with good data. And the right combination of data can lead to actionable steps. For the fullest picture, couple your data with administrative claims data, publicly available data, proprietary databases and science- or evidence-based care.
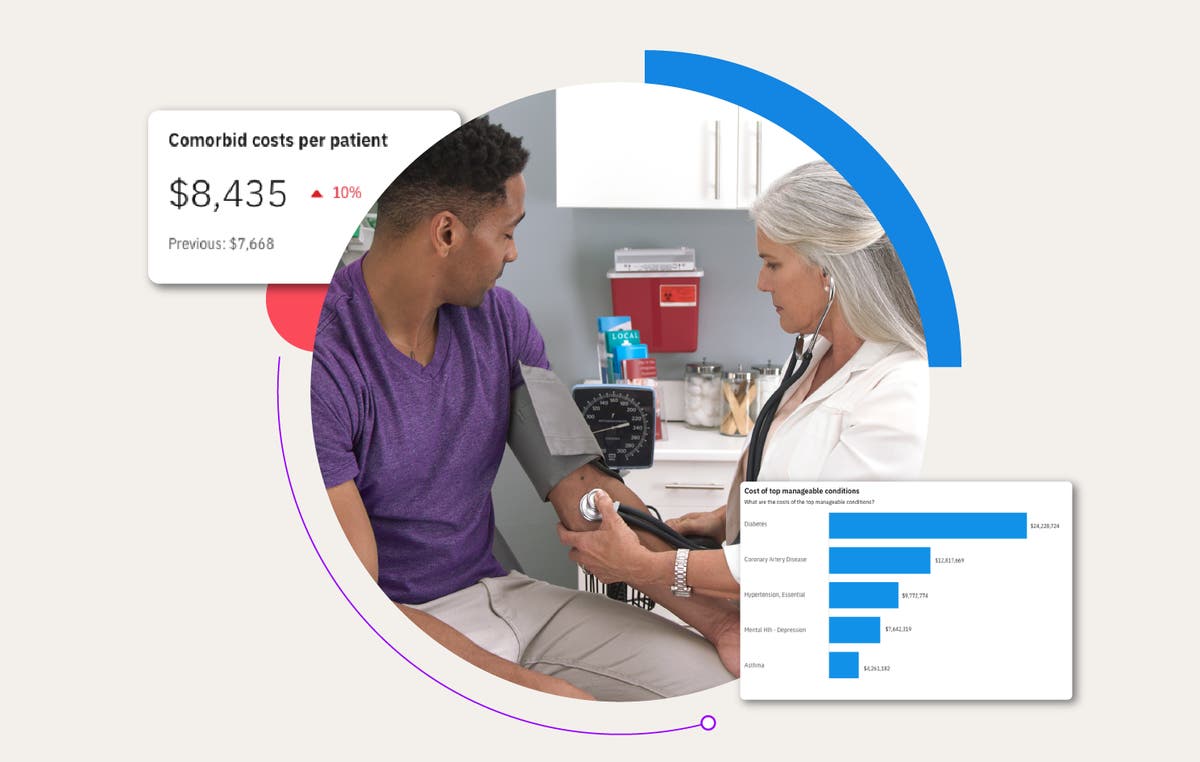
Truven by Merative can help you create a health equity dashboard to capture and visualize key metrics, which is a necessary part of the data and evidence analytics process. For your organization’s dashboard:
- Look for specific measures that have potential to drive positive change towards health equity and well-being.
- Identify and select specific, relevant metrics that are based on the data and evidence that you have curated and that are aligned with the needs of communities.
- Ensure you can effectively collect and track these metrics over time.
- Ensure measurements are useful and meaningful for the patients and communities; and can be tied back to the data and build on the evidence.
But the work doesn’t stop there. Data is continuously evolving, and as time progresses you need to consider additional fields to add to your datasets. For example, as gender identities and sexual orientation continue to expand, so should your data management fields. That’s why we not only help you stand up a dashboard with Health Insights, but we also are committed to helping you maintain that dashboard. Whether it’s through the addition of new fields or analytics.
Learn how healthcare analytics can help you get a better view of your population.
Step 3: Collaborations can maximize impact
The possibilities for partnerships and for collaborations to promote health equity are endless. They are limited only by the kinds of partnerships we choose. Community collaborations are also key.
Note that misconceptions about SDoH and data impact strategy decisions. Organizations can sometimes have a misunderstanding of the full range of the social factors that are relevant. Categories such as employment, economic stability, nutrition and housing play a major role. But there are also categories of social health, such as isolation and loneliness, that are increasingly becoming a major determinant of health. Individuals with social isolation, for example, suffer highest rates of poorer health outcomes, chronic conditions, depression and cognitive decline. Since physical, mental and social health are connected, we should also tackle this epidemic of social isolation for its role in health. We should also look for other hidden conditions, conditions data can help uncover.
Research suggests personal well-being is overwhelmingly driven by the non-medical factors that comprise SDoH.¹ Truven can supplement your clinical and other data sources with environmental and neighborhood data, integrating SDoH into Health Insights to provide a more rounded picture of population health:
- Understand how risk factors vary among communities where members live and how those factors impact health equity.
- Compare various segments of your population side by side, using aggregated data.
- Improve population health through increased engagement and tailored plan design.
- Analyze lifestyles and behaviors that impact care decisions and adherence to treatment.
- Identify at-risk populations with social needs who may face further health equity challenges, and design programs to target those needs.
- Utilize pre-defined Health Insights metrics, like anxiety, and slice it down to the segment level, such as race, gender identity, or ethnicity.
- See how your data compares to other organizations with benchmarking data.
As stakeholders with access to different sources of data, we are all in a unique position to collaborate and develop successful strategies that will impact positive health and outcomes. With clear definitions, measurable goals and strategic collaborations, we can play a role in helping all individuals achieve their optimal health.
Are you ready to address your population’s SDoH and overcome health inequities? Collaboration is the key.
Let’s chat.
Sources:
Hood, C. M., K. P. Gennuso, G. R. Swain, and B. B. Catlin. 2016. County health rankings: Relationships between determinant factors and health outcomes. American Journal of Preventive Medicine 50(2):129-135. https://doi.org/10.1016/j.amepre.2015.08.024
Related Articles
How healthcare analytics help employers reduce costs and improve employee health
Year after year, employers grapple with rising healthcare costs that feel beyond...
By Jennifer Huyck | 4 min. read

Morgan Health invests in Merative
Today, Morgan Health announced its investment in Merative as part of its mission to...
By Merative | 1 min. read

The missing puzzle piece: Linking MarketScan claims data with Veradigm EHR data
This new healthcare database unlocks the whole picture of patient care at an...
By Marcy Tatsch | 2 min. read
Ready for a consultation?
Our team is ready to answer your questions. Let's make smarter health ecosystems, together.
