Control costs and improve outcomes through site of care optimization

Healthcare costs continue to skyrocket. According to the National Business Group on Health 2025 Survey, healthcare costs are expected to increase 8% in 2025. This is the highest annual rate in the last decade and caps off a cumulative 50% increase since 2017. As we all know, there are many factors driving this such as inflation, rising prescription drug costs, medical technology and pharmacological advancements and innovations, provider consolidations, and increased chronic condition prevalence, to name a few. With these factors, there are also many strategies to put into place to mitigate costs including focusing on population health, new benefit designs, value-based care, payment integrity, price transparency tools, and many others.
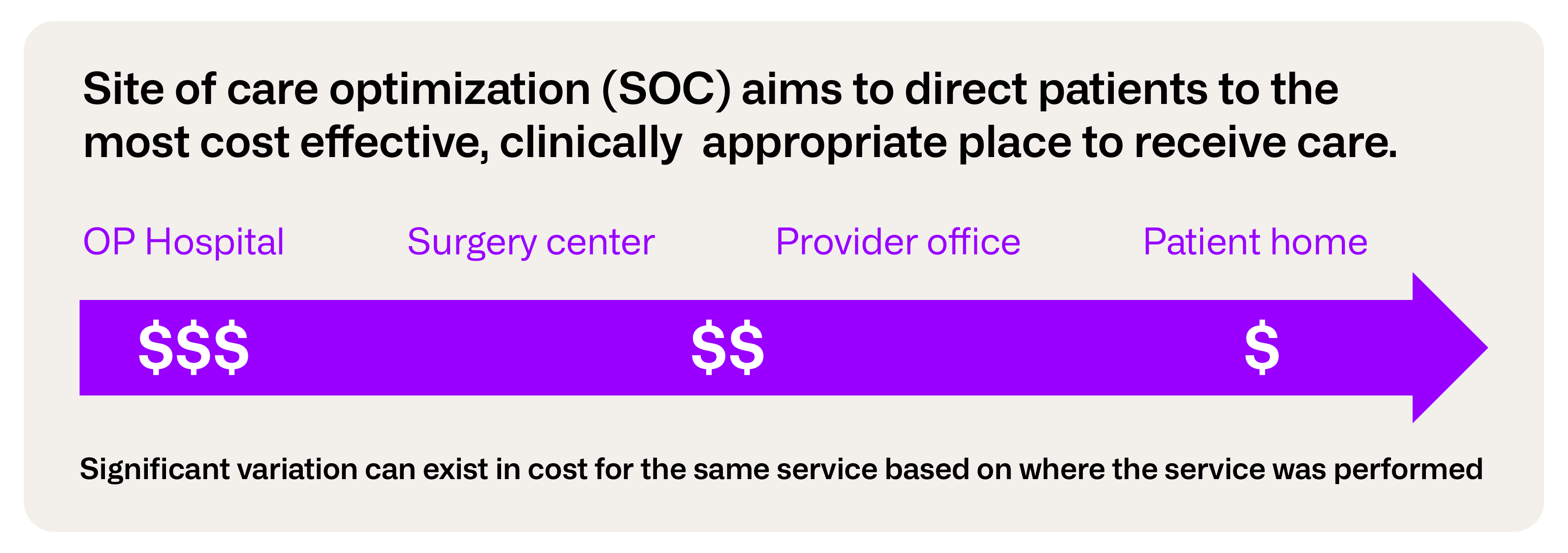
One strategy that gained steam during the COVID-19 pandemic and has remained a top opportunity, where data supports real savings potential, is Site of Care Optimization.
Site of Care Optimization is a broad-based strategy designed to improve efficiency in the delivery of healthcare by identifying the most cost-effective and clinically appropriate location for delivering health care services to patients.
There has been an ongoing shift in services traditionally concentrated in the inpatient care setting to outpatient settings and payers continue to evaluate their data and broader market trends to identify opportunities for additional savings while continually improving care and patient outcomes. According to a study by the Advisory Board tracking 15 high-risk procedures since 2017, 14 procedures have shifted to lower acuity settings and of those, 11 saw quicker shifts from 2019 to 2022, led by joint replacements. In the outpatient setting alone, comparable procedures may have significantly lower costs when performed in an office or ambulatory surgical center as compared to hospital onsite outpatient clinic.
Why site of care optimization matters
As an illustrative example, let’s discuss Benjamin, John, and Rolando who live in Mecklenburg County, North Carolina and had preventive colonoscopies in 2024. They have different primary care physicians and following their wellness checkup they received instructions to schedule the procedure. Their costs were as follows:

We can see there are significant pricing differentials between each of the locations, particularly the Outpatient Hospital Facility. Had Benjamin and John been referred to Ambulatory Surgical Center B and their colonoscopies cost the same as Rolando’s, the plan sponsor could potentially save $3,965 between the two. The plan sponsor analyzed their data for cost variations of preventive colonoscopies in Mecklenburg County and how that impacts their overall healthcare costs. Their members had 388 preventive colonoscopies with just over $1M in net payment.

A broader strategy that steers 25% (34 patients) of Outpatient Hospital preventive colonoscopies to ASCs could provide over $112K in potential savings based on average net payment. The plan sponsor also found of the 253 colonoscopies occurring in ASCs, 37% had costs higher than average, offering additional opportunities to shift colonoscopies already occurring in a lower acuity setting to lower cost ASCs.

Getting started: considerations for site of care optimization initiatives
Define areas of focus
The first key consideration in the process of any site of care initiative is identifying services that offer meaningful opportunities for savings and efficiencies. Top candidates would require significant utilization, meaningful pricing differentials by site of care, and impactability, including patient preference. Review of these procedures should focus on service settings, such as ambulatory surgical centers, outpatient hospitals, and surgeons’ offices, to identify settings with advantageous pricing in one relative to another. Business analysts must evaluate the service settings, procedures, patients, providers, and markets to focus on.

One example would be outpatient services highlighted above regarding preventive colonoscopies. Ideally, one would prefer to focus on highly utilized, relatively high-cost procedures offering the greatest savings and minimizing potential for negative patient outcomes. When seeking preventive care such as colonoscopy, mammogram, or non-emergent imaging for example, there may be little difference in the result based on the service setting for healthy patients. Advanced imaging performed in an outpatient hospital can be on par with the quality of those performed in an office or standalone outpatient facility. Another consideration in service selection is the current utilization of various sites of service and the potential to move those to lower acuity settings.
When looking at Merative’s MarketScan data for preventive colonoscopy costs, opportunities to optimize are easily spotted. The data show 34% of colonoscopies are being performed in the Outpatient Hospital setting, which on average cost 44% more than ASC sites based on the U.S. MarketScan Commercial under 65 population.

Another consideration in the selection of services is network adequacy. The provider environment and network in each geographic area will have an impact. When there are relatively few options available to obtain a given service, the challenge of finding a willing provider or identifying sites to offer efficient care options would limit the feasibility of migrating patients to other service settings. This underscores the importance of network management and provider partnerships to advance site of care optimization.
Analytic groupers
As payers seek to shift care to more cost-efficient settings, robust data and meaningful analytics are necessary to ensure success. When evaluating data to determine a suitable target for care optimization efforts, it is important to capture the full cost of a procedure. This can be complicated by the fact that contract terms and billing practices vary across the provider landscape. In the example of the preventive colonoscopies, various ancillary services may be included in a given event and can often have an impact on the final cost.

If we look back at Benjamin, John and Rolando and take a closer look at their cost, we can see that had the plan sponsor focused solely on the anchor procedure of colonoscopy, it would have painted a much different picture. While Ambulatory Surgical Center B continues to look like the most efficient option, the Outpatient Hospital Facility looks more efficient as compared to Ambulatory Surgical Center A for the anchor procedure alone because the ancillary services drove the bulk of overall cost. It is important for payers to utilize analytic methodologies and groupers that can accurately join seemingly disparate claims related to the primary procedure for this reason.
However, even for less complicated procedures, some patients may still be best served in a higher acuity setting based on their individual risk profile and severity of their clinical episodes of care, so clinical context should always be evaluated.
Robust datasets
Another way to assess market opportunities for site of care optimization efforts is to recognize where your goalposts are located. The healthcare market is ever-changing; never stagnant. Drivers of change including legislative policies at the federal, state and local level, emerging treatments and new diagnostic technologies, and mergers and acquisitions across the entire healthcare landscape pose challenges. Understanding your market and what is reasonable for site of care optimization targets (e.g. for procedure x what is a reasonable target for ASC as compared to OP Hospital), as well as reimbursement targets, requires data.
Reimbursement Benchmarks can surface deep insights on paid reimbursement amounts for a given procedure in a specific market across various sites of care, providing necessary insights into the variation in reimbursement in your market(s) of interest. In addition, reimbursement benchmarks should include multiple types of benchmark groupings for CPT/HCPCS, ranging from focusing only on the reimbursement for the primary procedure to determining how the reimbursement is impacted if the procedure is included as a case rate with its associated ancillaries. Strong and reliable benchmarks will provide necessary data for your site of care analysis, mitigate risk, and defend your pricing targets during site of care optimization negotiations.
In the above colonoscopy example, if the plan sponsor wanted to better understand the strength of their networks in the Charlotte, NC market of Mecklenburg County, reimbursement benchmarks can provide accurate data points for contract negotiations and site of care assessment. In the example below, MarketScan’s Reimbursement Benchmarks data was used to demonstrate the variation in reimbursement for colonoscopies in Charlotte, NC. The tables below illustrate reimbursement for both the primary procedure and the total case rate which includes ancillary reimbursement.

When looking at the ASC costs across percentiles, we see that case rates are comparable to the primary procedure cost. This is not true for the OP Hospitals, which offer significantly more opportunities for savings by shifting to ASCs, even at the 75th percentile. Case rate reimbursement at the 50th percentile provides potential savings of approximately ~$1,400 per procedure, while case rates at the 75th percentile yields a potential savings of ~$3,400 per colonoscopy. It is important to understand the type of contract (e.g. fee for service or case rate) you have in place with your carrier, but also how much volume there is to shift.
Conclusion
Health plans and employers interested in pursuing site of care optimization as a means of controlling costs and improving outcomes need strong and reliable data to shape strategy, steer members, and successfully negotiate contracts. By identifying services that yield meaningful opportunity, understanding the nuances of reimbursement amounts, and having reasonable price and quality goals, the odds of successfully implementing a site of care optimization strategy or engaging suitable provider partners improve.
If you are interested in learning more about how Truven can help your organization with healthcare analytics and member engagement, schedule a chat.
Related Articles

Unlocking real-time insights: how on-demand analytics reduces latency for faster decision-making
When it comes to data-driven decision making, analytic latency can have a major...
By Kristen Hutchins | 5 min. read

Maximize your insights: What happens when analytics algorithms are interconnected?
Data is arguably a company’s greatest asset. But that data is insignificant if you...
By Matt Warner | 4 min. read

Optimizing value-based healthcare: 5 strategies for effective provider network management
In today's rapidly evolving American healthcare industry, the collaboration between...
By Brandi Hodor | 6 min. read
Ready for a consultation?
Our team is ready to answer your questions. Let's make smarter health ecosystems, together.
